Scoliosis
What is scoliosis?
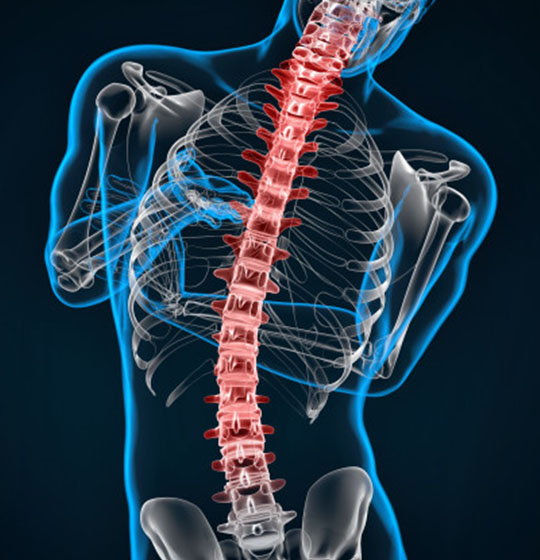
Scoliosis is a disorder that causes an abnormal curve of the spine, or backbone. The spine has normal curves when looking from the side, but it should look straight when looking from the front. People with scoliosis develop additional curves to either side, and the bones twist on each other like a corkscrew. Scoliosis is about two times more common in girls than boys. It can be seen at any age, but it is most common in those over 10 years of age.
What causes scoliosis?
In most cases, the cause of scoliosis is unknown (idiopathic). This type of scoliosis is described based on the age when scoliosis develops. If the patient is less than 3 years old, it is called infantile idiopathic scoliosis. Scoliosis that develops between 3 and 10 years of age is called juvenile idiopathic scoliosis, and patients that are over 10 years old have adolescent idiopathic scoliosis.
There are two other types of scoliosis:
Functional: In this type of scoliosis, the spine is normal, but an abnormal curve develops because of a problem somewhere else in the body. This could be caused by one leg being shorter than the other or by muscle spasms in the back.
Neuromuscular: In this type of scoliosis, there is a problem when the bones of the spine are formed. Either the bones of the spine fail to form completely, or they fail to separate from each other. This type of scoliosis develops in patients with other disorders including birth defects, muscular dystrophy, cerebral palsy, or Marfan’s disease. This type of scoliosis is often much more severe and needs more aggressive treatment than other forms of scoliosis.
How is scoliosis diagnosed?
If you think you have scoliosis, you can attend our chiropractors for an examination. The chiropractor will ask questions including if there is any family history of scoliosis, or if the patient has had any pain, weakness, or other medical problems.
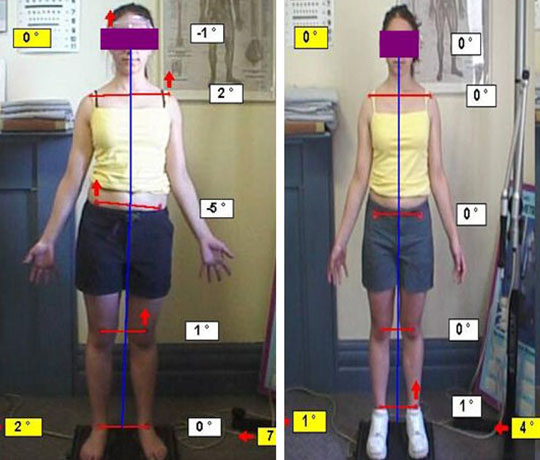
The examination involves looking at the curve of the spine from the sides, front, and back. The patient will be observed from the waist up to see if any abnormal curves are present. The patient will then bend over trying to touch their toes. The chiropractor will also look at the symmetry of the body to see if the hips and shoulders are at the same height. Any skin changes will also be identified that can suggest scoliosis is due to a birth defect.
The more growth that a patient has remaining increases the chances of scoliosis getting worse. As a result the chiropractor may measure the patient’s height and weight for comparison with future visits. Other clues to the amount of growth remaining are signs of puberty such as the presence of breasts or pubic hair and whether menstrual periods have begun in girls.
If the chiropractor believes you have scoliosis, you could either be asked to return for an additional examination in several months to see if there is any change, or the chiropractor may take x-rays of your back. If x-rays are obtained, the chiropractor can make measurements from them to determine how large of a curve is present. This can help decide what treatment if any is necessary. Measurements from future visits can be compared to see if the curve is getting worse.
Scoliosis Treatment Using a Combination of Manipulative and Rehabilitative Therapy: A Retrospective Case Series
FROM: BMC Musculoskeletal Disorders 2004 (Sep 14); 5: 32 ~ FULL TEXT
Mark W Morningstar, Dennis Woggon, and Gary Lawrence
Pettibon Biomechanics Institute 3416-A 57th St Ct. NW; Gig Harbor, WA 98335, USA
Background The combination of spinal manipulation and various physiotherapeutic procedures used to correct the curvatures associated with scoliosis have been largely unsuccessful. Typically, the goals of these procedures are often to relax, strengthen, or stretch musculo tendinousand/or ligamentous structures. In this study, we investigate the possible benefits of combining spinal manipulation, positional traction, and neuromuscular re-education in the treatment of idiopathic scoliosis.
Methods A total of 22 patient files were selected to participate in the protocol. Of these, 19 met the study criterion required for analysis of treatment benefits. Antero posterior radiographs were taken of each subject prior to treatment interventionand 4?6 weeks following the intervention. A Cobb angle was drawn and analyzed on each radiograph, so pre and post comparisons could be made.
Results After 4?6 weeks of treatment, the treatment group averaged a 17°reduction in their Cobb angle measurements. None of the patients’ Cobb angles increased. A total of 3 subjects were dismissed from the study for non compliance relating to home care instructions, leaving 19 subjects to be evaluated post-intervention.
Conclusions The combined use of spinal manipulation and postural therapy appeared to significantly reduce the severity of the Cobb angle in all 19 subjects. These results warrant further testing of this protocol.
ASSESSMENT OFFER
For the price of a standard consultation ($45) our doctors with 25 years of clinical experience will assess your scoliosis, clinical history and X-Rays. They will provide an opinion whether their specialized conservative treatment and exercise program can reduce the scoliosis and prevent possible surgical intervention. Our doctors work closely with orthopaedic surgeons to provide a comprehensive care plan. Ring our clinic on 9326-1755 and arrange an appointment.
Forward Head Posture
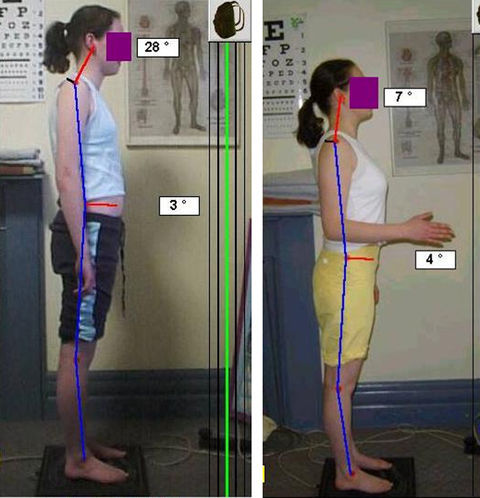
Forward head posture is a clinical entity that has been identified by multiple authors as a significant factor in a variety of musculoskeletal pain syndromes. Forward head posture is the most common cause of the tension headache syndrome. Forward head posture is an increasingly common problem of the 21st Century. Adolescents develop forward head posture from extended computer use, especially laptop computer use. Extended usage of computers leads to the head moving forward of the shoulders resulting in the anterior (front) muscles of the neck becoming weak. This type of posture puts stress on the posterior neck and upper back muscles resulting in increased tension. This posture over time leads to chronic pain and headaches in patients as young as their late teens.
Forward Head Posture doubles the load on the cervical spine and also causes the shoulders to roll forward making the shoulder tendons more vulnerable to wear and tear. Poor posture and body mechanics may cause early disc degeneration and osteoarthritis. Forward Head Posture causes a number of effects on the body
Posture – Influences Breathing
Posture influences a person’s ability to breath. The forward head posture encourages shallow breathing because the ribs and diaphragm can no longer move properly. As a result, the accessory respiratory muscles connecting from the neck to the upper ribs – normally used as a safety reserve during vigorous exercise – become activated.
This creates abnormal tension in the muscles and soft tissues, and what normally would be relaxed becomes tight and what would normally tighten and relax becomes inactive and weak.
Posture – Changes Muscle Tissue
Poor posture can change muscle tissue and cause tightness, pain and tenderness, as well as weakness. Characteristic symptoms may be present according to which muscles are involved (i.e. trigger points, scalene syndrome and pect minor syndrome).
Posture – Effects How Muscles Work
Many rehabilitation specialists and neurologists believe that when injured our body adopts certain movement patterns where some muscles become overactive and tight while others become inactive and loose. These patterns are related to the normal development of motor control. What has been found is that when injured the earlier more primitive movement patterns dominate while the later more complicated activities become inhibited.
An extreme example of this feature is a person who has had a stroke – there is a well recognized pattern of certain muscles becoming tight while other muscles become weak. The characteristic pattern for postural dysfunction in the neck and upper back has been called an Upper Crossed Syndrome. There is a classic pattern of chin forward posture, tight trapezius muscles and weak deep neck flexor muscles.
Posture – Influences The Nervous System
Faulty posture can trap or irritate nerves. Local mechanical irritation can cause nerves to fire inappropriately – creating an – Abnormal Impulse Generating Site – in the same way rubbing the insulation off an electrical cable may cause a short circuit. For example, slouching may cause pain and a burning sensation in the middle back – Notalgia paraesthetica -because the nerves travel along a curved path through the muscles. If you change the length and alignment of the muscles, the nearby nerves may become vulnerable to physical stretch and become irritated.
Poor posture is a very common underlying cause of spinal dysfunction. The spine has a rich nerve supply and poor function can give characteristic symptoms: disturbances in the upper cervical spine may contribute to headaches and balance disorders, disturbances in the upper back area can cause headaches, chest discomfort and pins and needles in the hands i.e. T4 syndrome.
One aspect of the nervous system that is often forgotten is that the brain relies on high quality information (sensation) coming back from the muscles and joints of the body. With poor posture the spinal joints become stiff, especially in the upper back region, and begin to provide less ‘input’ back to the brain. With less input the brain can gradually lose awareness of that area and begins to think of that area as a solid block rather than individual segments. This change of awareness leads to a further loss of movement.
Posture – Causes Tissue Creep
Poor posture can lead to tissue creep. That is when the collagen fibres in the inner fabric of ligaments stretch and deform – similar to how plastic gives way under stress. Once this change has happened, it is difficult for the tissues to return to their normal length. Tissue creep may occur after long or repeated loading – it can start after as little as 15 minutes of slouching. This commonly effects people who spend hours working in the one position. Children who play computer games for long periods are at risk of tissue creep.
This common problem can be avoided by recognising the forward head posture in adolescents and retraining their muscles with advice from Chiropractors trained in rehabilitation.
In the graphic on the left, the first sketch (shown top-left) represents “perfect” head posture. A line dropped from the center of the ear would land directly in the center of the shoulder. The photograph on the right demonstrates someone with moderately severe forward head posture.
For every inch your head moves “forwards”, the head “gains” 2.5 kilos in weight, as far as the muscles in your upper back and neck are concerned, as they have to work harder to keep the head (chin) from dropping forwards onto your chest. This forces the muscles that raise the chin to remain in constant contraction, putting pressure on the nerves at the back of the skull and reduces normal venous drainage from the muscles of the skull. This causes headaches at the base and front of the skull, and even mimic sinus headaches!
Persistent forward head posture (a.k.a ?hyperkyphotic posture?) puts compressive loads upon the upper thoracic vertebra, and is also associated with the development of Upper Thoracic Hump, which can evolve into Dowager Hump when the vertebra develop compression fractures (anterior wedging). A recent study found this hyperkyphotic posture was associated with a 1.44 greater rate of mortality.
It’s not uncommon to observe 2″ of anterior head placement in new patients. Would you be surprised that your neck and shoulders hurt if you had a 10 kilo watermelon hanging around your neck? That’s what forward head posture is doing to you! Left uncorrected, FHP will continue to decline. Chiropractic can be very effective, especially in the hands of a chiropractic rehabilitationist. Our specialty is in reversing joint fixations (subluxations) and in re-invigorating the muscles that retract the head.